Over the next few weeks, I’m going to be sharing some of my past most-loved-content. The post below is an updated version of one of my most popular blogs from 2015.
Today I want to talk about something that is rather common in women. It’s more likely to naturally happen as women get into your 30s and 40s, but can also occur at a younger age.
What I am referring to is anovulatory cycles, which is where you get your period even though you haven’t ovulated.
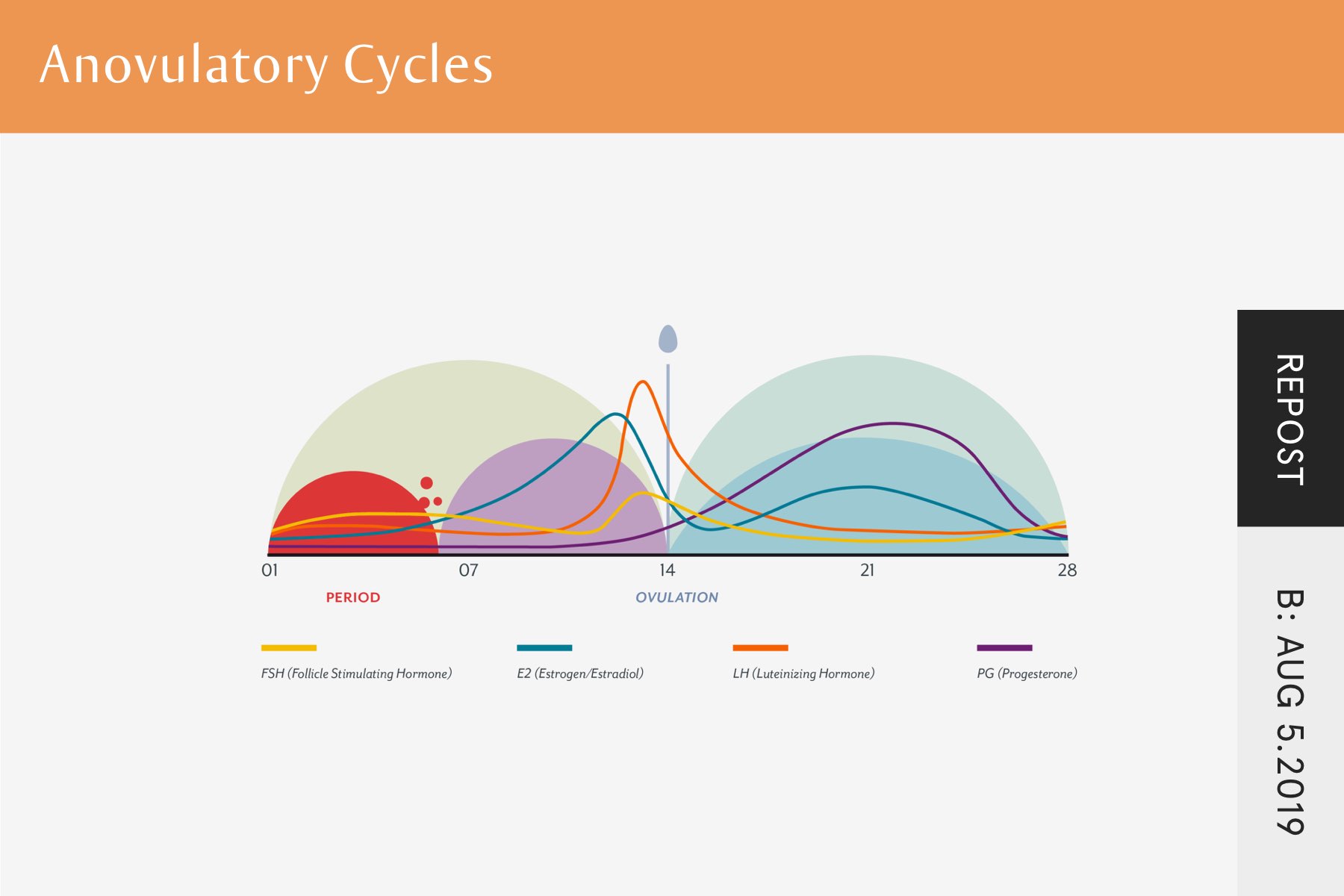
A woman’s cycle can be broken into two phases. Let me use a standard 28-day cycle as an example, even though cycles can be shorter or longer than this.
The first two weeks are known as the follicular stage as this is about building up the follicle, which is where the egg is housed.
The second two weeks are known as the luteal phase and the focus here is on continuing to build up the endometrium. This is the layer of blood and nutrients that cover the uterus; if conception is to happen, this is where the fertilised egg will embed.
And right in the middle of these two phases is where you have ovulation. This is where the egg is released from the follicle and makes its way from the ovary into the fallopian tube.
An anovulatory cycle is where you have the follicular and luteal phase without the ovulation in the middle
Most women have no idea when this is happening.
For someone who pays attention to their various ovulation symptoms – like changes in cervical mucus, cervix position, body temperature, libido, breast tenderness, bloating – it can be fairly clear when ovulation has occurred.
But most women aren’t paying this kind of attention to these rhythmical body changes, so any symptoms of not ovulating are missed or simply chalked up to being part of the normal cycle.
It’s typically only when a woman is failing to become pregnant and investigation occurs that they find out.
Now you may be thinking, so what’s the big deal? If I’m not trying to get pregnant, and I’m not ovulating, why does it matter?
Well, it matters for several reasons.
The first is that having anovulatory cycles can be the cause of some of the menstrual symptoms you are suffering with. To understand this, let me explain a small part of how your cycle works.
At the point of ovulation, the egg is released and leaves behind the sack that was previously housing it. This sack, known as the corpus luteum, is what produces high amounts of progesterone in the second half of the cycle. If you don’t ovulate, you don’t get this increase in progesterone.
Low amounts of progesterone can be associated with a whole host of reproductive symptoms. Migraines, cramps, blood clots, hair loss, fatigue, and lots more. So while someone may not be trying to get pregnant, they probably do care about these symptoms if they’re getting them.
And typically if ovulation isn’t occurring, it’s not just progesterone that is low. So are luteinising hormone (LH), oestrogen, and potentially follicle stimulating hormone (FSH).
While these hormones are typically thought of as “reproductive hormones”, they have many functions outside of reproduction. And this is the second reason you want to avoid anovulatory cycles.
When we think of a woman’s cycle, it’s common to see it purely for procreation. Some women will be having irregular cycles or no cycles at all and think that it isn’t something to worry about because they don’t want to have kids or at least not at the moment. They’re told that it’s something to fix at the point of deciding they now want to get pregnant.
Well, a woman’s cycle has lots of benefits outside of reproduction. This is largely because of the hormones that are released throughout the cycle.
For example, oestrogen outside of reproduction has an impact on cell growth, blood vessels, wound healing, memory, and bone health (to name just a few of its roles).
Progesterone, another “reproductive hormone”, impacts on nerve function, bone and skin health, thyroid function, immune activity, and mood (again, just to name a few of its functions).
This means that these hormones are having an impact on all your body systems.
As I mentioned, most women who are having anovulatory cycles have no idea it is happening.
Especially as women age, anovulatory cycles can become more common. But rather than ovulation completely stopping, what often happens is that it becomes more irregular. So one cycle you’ll ovulate, the next one you won’t.
There are several ways that you can check whether you’ve ovulated. Some you’ll need a doctor for, some you can do at home.
If you want to go down the blood test route, there are two potential tests you can do.
One is testing hormones just before the midpoint of your cycle. Somewhere around 24-48 hours before you think ovulation should occur. Just before ovulation occurs you get an increase or surge in a hormone called Luteinizing Hormone or LH. It is this surge that causes ovulation.
So if you have a cycle that is about 28 days, and day one is the first day of your period, this would be getting tested around day 12 or 13. This isn’t exact, as you can have a shorter or longer first half of the cycle, so you may want to also pay attention to other symptoms (see below).
With the blood test for LH, there isn’t consensus around what would be the cut off point that would guarantee ovulation. But according to this study (hat tip to Nicola Rinaldi for making me aware of it), it should be somewhere around 15 IU/L, potentially 20 IU/L to be on the safe side. And then if you are seeing numbers higher than this, ovulation is likely to have occurred, at least with this particular cycle.
LH can be elevated outside of ovulation, particularly in Polycystic Ovary Syndrome (PCOS). So it can be worth also checking hormone levels in the early part of the cycle, say around day 3 or 4, to see what the baseline levels are before the surge at the midpoint.
The other blood test you can do is for progesterone. As I mentioned earlier, progesterone is produced from the sack that is left behind after ovulation, called the corpus luteum. If ovulation occurs, progesterone will increase. If it doesn’t, it will stay low.
Officially this test is meant to be done at seven days past the point of ovulation. But I think it is fine at any point in the second half of the cycle that is not too close to ovulation or menstruation starting. A progesterone level of 5ng/ml probably indicates ovulation has occurred, but ideally, it would be 10ng/ml or above.
Combining both of these tests can be a good way of checking to see if ovulation has occurred.
The next method is something you can do at home.
To excrete hormones, one of the methods the body uses is through urination. And the levels of hormones in the body will impact on the amount being excreted in the urine.
This method involves urinating on test strips that can detect the levels of LH or LH and oestrogen (depending on which product you use). This testing is done around the midpoint of the cycle, and the test strips are detecting whether there has been a surge in hormones, where the levels would be higher.
This method is great because it can be done at home every month and is relatively inexpensive.
The big drawback is to do with accuracy. And this is especially true if someone is on the low end, where they are on the cusp of potentially having enough hormones to create ovulation. It can be hard to decipher if ovulation has occurred and this can be rather maddening.
It’s unlikely to give a false positive, so if it clearly shows that ovulation has occurred, it’s pretty trustworthy. But it is more likely to give false negatives, when hormone levels are low but ovulation has occurred.
Symptom Changes
The final method to gauge if ovulation has occurred is by paying attention to various body changes.
While it may not have the gold standard of a blood test, when many symptoms are paid attention to (and someone has learnt to do this properly) it can be very accurate.
This is a big topic so I’m going to pick a couple of examples of things to pay attention to. For these indicators to be an accurate feedback mechanism, you need to be paying attention all month long to notice how symptoms change, not just at the points I’m mentioning below:
For more detail on these and a list of other symptoms connected to ovulation, you can check out this article.
Anovulatory cycles are part of our evolutionary history. Bringing a human into the world is a huge calorie demand on the human body.
Historically, at different points in the seasons or when food was harder to come by, it made sense for the body to prevent ovulation as it wouldn’t be the right time to get pregnant.
But given the environment that we now live in (at least in the West), this should be occurring infrequently, especially in women below 30. And when it is happening, it’s typically connected to dietary and lifestyle factors and is definitely correctable.
I’ve had many clients where this was a problem and was leading to an inability to conceive. From working together, they were able to get pregnant.
While this article is specifically focused on anovulatory cycles, I help women deal with many aspects relating to menstruation and reproductive health. Issues like difficulty conceiving, irregular or absent periods, and cycles and periods that are filled with negative symptoms.
If there is one take-home message I want you to get from this, it’s that your cycle is much more important than just procreation. Many of the hormones involved have a body-wide impact and so improving your cycle isn’t just about increasing fertility or improving menstrual symptoms, it’s about improving health in general.
I’m a leading expert and advocate for full recovery. I’ve been working with clients for over 15 years and understand what needs to happen to recover.
I truly believe that you can reach a place where the eating disorder is a thing of the past and I want to help you get there. If you want to fully recover and drastically increase the quality of your life, I’d love to help.
Want to get a FREE online course created specifically for those wanting full recovery? Discover the first 5 steps to take in your eating disorder recovery. This course shows you how to take action and the exact step-by-step process. To get instant access, click the button below.
Discover the first five steps to take in your eating disorder recovery.
Get started the right way and be on the path to full recovery and the freedom it will bring YOU.
Unlike other approaches focusing on just one aspect of recovery, this course shares a framework that demonstrates what full recovery is really about and gives you the tools to get there.
Get Instant Access!
Share
Facebook
Twitter